Things are getting sticky for the country’s healthcare system in 2026.
Costs are continuing to rise, access to care remains uneven, and both patients and employers are feeling the strain of a system that is growing more expensive and complex. Current projections suggest U.S. medical costs will increase another 9–10% this year, pushing healthcare affordability back to the center of the national conversation.
This isn’t a sudden shift. It’s the continuation of a trend that’s been building for years, but 2026 may be the year it finally becomes impossible to ignore.
Rising Costs Are Changing How (and Whether) People Seek Care
With 60% of Americans skipping medical visits to save money, there’s a growing disconnect between the American healthcare system and the people it’s meant to serve.
When patients delay or avoid primary care because of cost uncertainty:
- Routine issues escalate into complex problems
- Chronic conditions go unmanaged
- Preventive care gets postponed
The result is a system that costs more over time while delivering less value to patients.
The Limits of an Insurance-First Model
For many patients, traditional insurance-based primary care has become difficult to navigate and even harder to budget for. Every year brings:
- Higher premiums
- Reset deductibles
- Out-of-pocket costs that feel disconnected from actual care
For employers, especially small and mid-sized businesses, offering health benefits has become a balancing act between affordability and coverage adequacy.
Each year brings higher costs and fewer options, while employees remain frustrated by limited access and confusing billing.
Simpler Care Models Are Getting More Attention
Because of this complexity, patients and employers alike are looking for ways to make everyday care:
- Predictable
- Transparent
- Easier to access
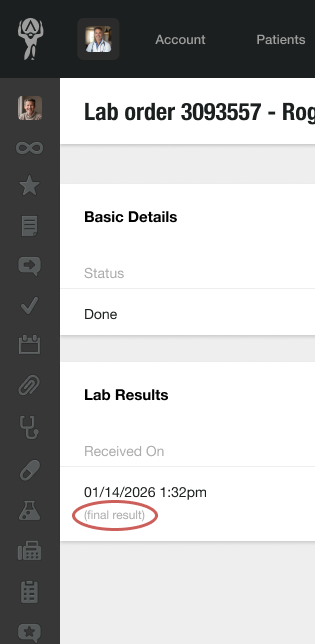
This is where membership-based primary care models, such as Direct Primary Care (DPC), are receiving renewed attention.
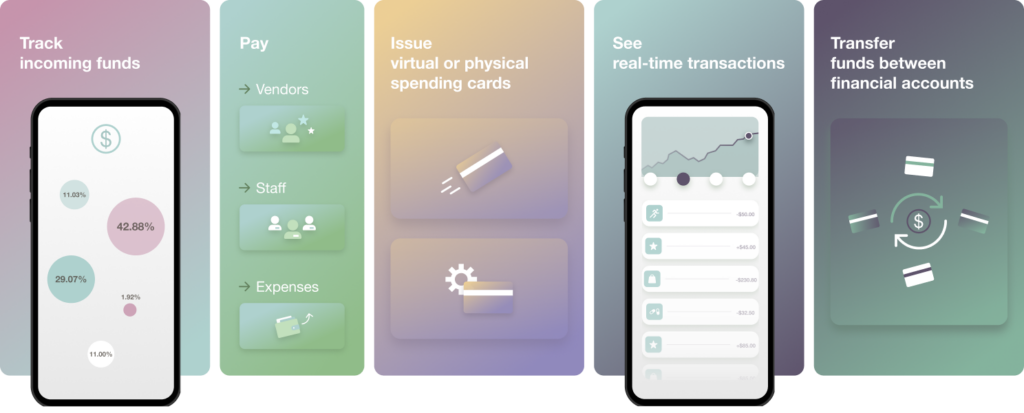
At its core, DPC offers a straightforward exchange: patients pay a flat monthly fee for primary care services, completely bypassing insurance bureaucracy, per-visit charges, and copays.
This structure not only removes the financial uncertainty that causes patients to hesitate before scheduling an appointment, but it also allows physicians to focus on care delivery rather than administrative overhead.
Physicians can spend more time with patients, reducing overwork and burnout and ultimately enabling a sustainable practice of medicine.
This shift is practical rather than ideological. When costs rise and access becomes more difficult, people look for models that are understandable and reliable.
The Growth of DPC Reflects Market Demand, Not Policy Mandates
There are now over 2,700 DPC practices operating in the U.S., with the broader market projected to approach $90 billion in the coming years.
This expansion hasn’t happened overnight. More importantly, it hasn’t been driven by large health systems or top-down government mandates. It’s happened gradually, as:
- Patients seek more accessible and affordable care
- Physicians look for sustainable ways to practice and avoid burnout
- Employers explore benefit structures that prioritize value over volume
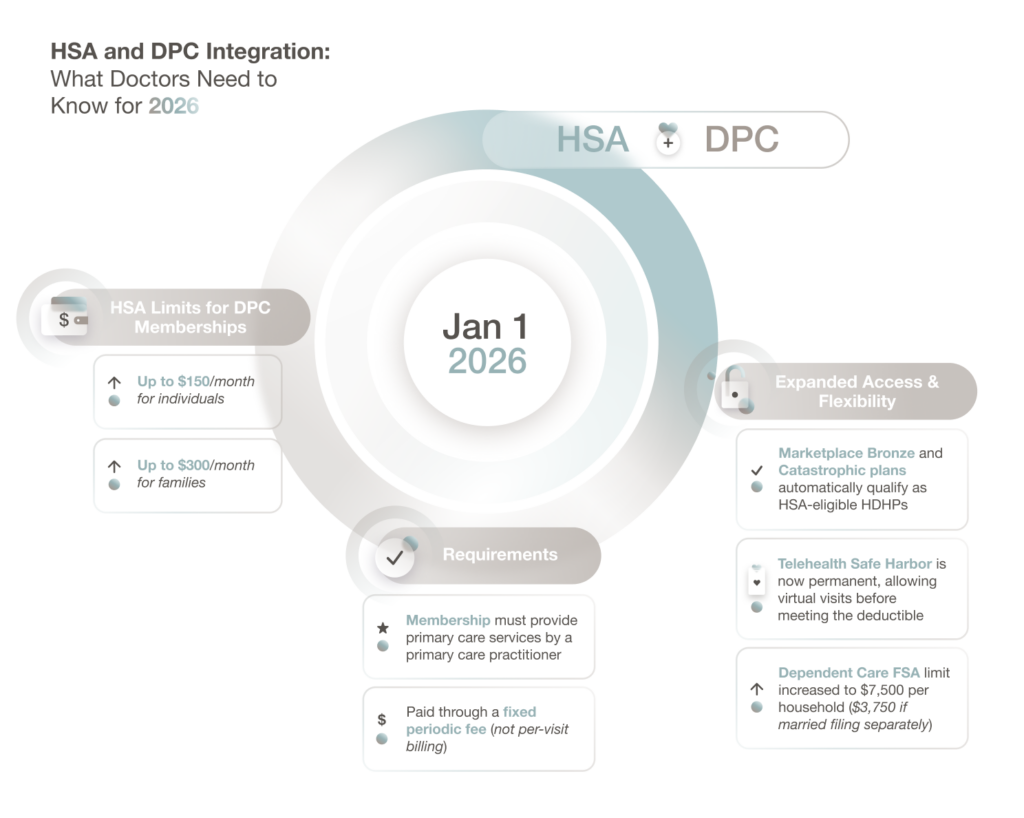
Regulatory shifts are also beginning to catch up. Recent federal changes, effective in 2026, allow patients to use HSAs for DPC memberships, removing a long-standing source of confusion and friction and making it easier for patients to pair Direct Care with high-deductible health plans.
Together, these factors suggest that 2026 won’t just be another expensive year for healthcare. It may be a year when more people actively question whether the traditional path still makes sense for everyday care.
What This Means for the Future of Primary Care
Health insurance isn’t going away. Catastrophic coverage, specialty care, and hospital services will always matter. But primary care was never meant to run through endless bureaucracy, and right now the market is correcting that mistake.
As costs rise, models built on predictable pricing, direct relationships, and easy access align more closely with how patients want to receive care. You only have to look at the steady growth of DPC practices to know that this isn’t a passing trend. It’s a response to a system that has priced families out and strained the doctor–patient relationship to the breaking point.
If 2026 becomes the most expensive year in healthcare history, it may also be remembered as the moment patients, employers, and physicians stopped accepting complexity as the norm—and chose a model that is simpler, more transparent, and easier to trust.
And that model is Direct Primary Care.